For Parents
We are a full-service pediatric office—caring for ages ranging from birth to 21.
Below is information on common pediatric healthcare concerns.*
Even if you don’t see a particular concern listed—please, contact us.
We want to help you and your child—no matter what their healthcare needs are!
Well-Child Exams
Read More
You know to take your child to a healthcare provider when they’re sick. But, pediatric healthcare visits are just as important when your child is healthy.
The American Academy of Pediatrics (AAP) suggests a schedule of well-child exams from birth through 21 years of age. Learn more about these visits and the Milestones that Matter to your child’s development.
It’s also worth familiarizing yourself with the Ages & Stages your child will progress through on their journey to adulthood. They are:
- Prenatal
- Baby (0–12 months)
- Toddler (1–3 years)
- Preschool (3–5 years)
- Grade School (5–12 years)
- Teen (12–18 years)
- Young Adult (18–21 years)
We also welcome visits with expecting parents—to see if our office will be a good fit for your family’s pediatric healthcare needs.
Lactation Support
Read More
The American Academy of Pediatrics (AAP) recommends breastfeeding as the sole source of nutrition for your baby for about six months. After that, as long as both mother and baby desire it, breastfeeding may be continued.
Learn more about how breastfeeding provides excellent nutrition, sets babies up for healthy growth and development, and benefits the mother.
If there is a medical reason you cannot breastfeed or you choose not to do so, you can still achieve similar feelings of closeness by rocking, cuddling, stroking, and gazing into your baby’s eyes during feeding—regardless of the milk source.
Before deciding on the issue, be sure you thoroughly understand the advantages and disadvantages of breastfeeding and bottle-feeding, and you are aware of all the options available to you.
Learn more about deciding to breastfeed or bottle-feed.
We are here to support you, too!
Common Cold
Read More
Your child probably will have more colds, or “upper respiratory infections,” than any other illness. Before the age of two, most children have eight to ten colds.
Colds are caused by viruses—which are much smaller than bacteria. A sneeze or a cough by someone with a virus can then be breathed in by another person, making them sick.
Signs and symptoms of a cold in children include:
- runny nose (first, a clear liquid coming out; later, a thicker, often colored mucus);
- sneezing;
- low fever (101–102 degrees Fahrenheit [38.3–38.9 degrees Celsius]), particularly at night;
- not wanting to eat;
- sore throat and, perhaps, difficulty swallowing;
- cough;
- fussiness on-and-off; and
- slightly swollen glands.
Note: Pus on the tonsils, especially in children three years and older, may mean your child has an infection called strep.
If your child has a typical cold without major problems, the symptoms should slowly disappear after seven to ten days.
Unfortunately, there’s no cure for the common cold. Antibiotics may be used to fight bacterial infections, but they do not affect viruses.
The best you can do is to make your child comfortable. Make sure your child gets extra rest and drinks water or other liquids.
Learn more about children and colds.
Learn more about caring for your child when they have a cold or the flu.
Learn more about how much fever and pain medicine to give your child.
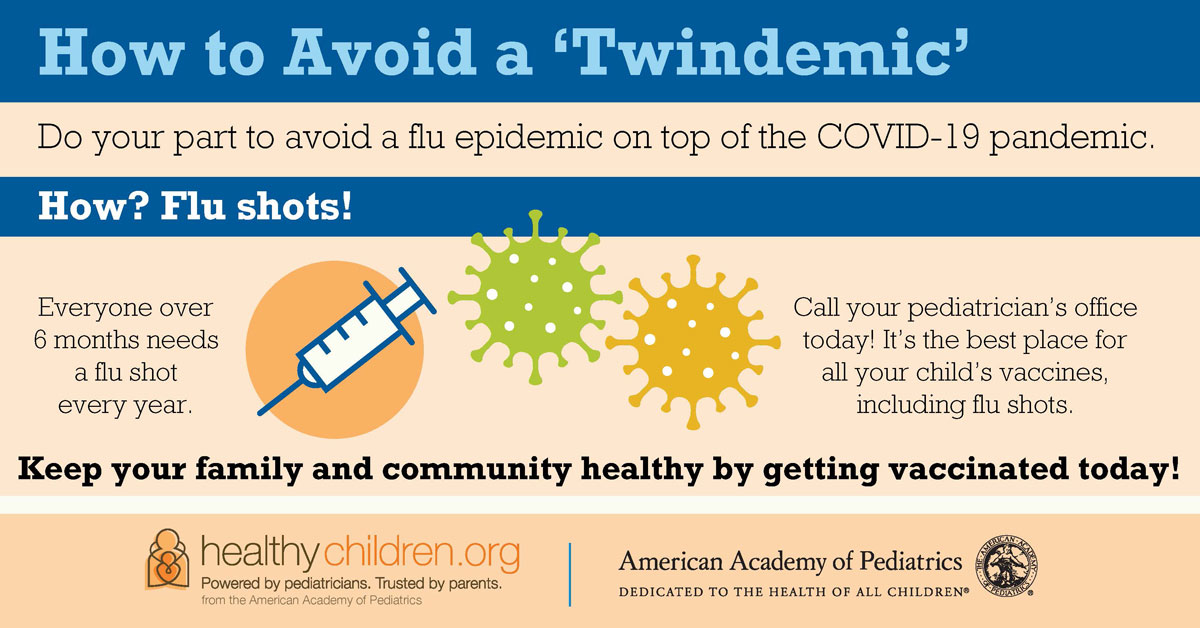
Influenza (Flu)
Read More
The flu (short for influenza) is an illness caused by a respiratory virus, and it can spread rapidly through communities.
When someone with the flu coughs or sneezes, the virus becomes airborne and those nearby can inhale it through their nose or mouth. The virus can also be spread when one touches a contaminated hard surface, such as a door handle, and then places his hand or fingers in his nose or mouth or rubs his eye.
Flu season usually starts in the fall and ends in the spring and tends to be most frequently found in preschool or school-aged children.
Flu symptoms include:
- A sudden fever (usually above 101°F or 38.3°C)
- Chills and body shakes
- Headache, body aches, and being a lot more tired than usual
- Sore throat
- Dry, hacking cough
- Stuffy, runny nose
- Nausea, vomiting, and diarrhea
After the first few days, a sore throat, stuffy nose, and continuing cough become most evident. The flu can last a week or even longer.
A child with a common cold usually has only a low-grade fever, a runny nose, and only a small amount of coughing. Those with the flu usually feel much sicker, achier, and more miserable.
Learn more about the flu.
Learn more about caring for your child when they have a cold or the flu.
Learn more about how much fever and pain medicine to give your child.
Parents can help their children prepare for flu season with the Ready Wrigley Prepares for Flu Season coloring book (in English or en Español) by the Centers for Disease Control & Prevention (CDC).
Pinkeye (Conjunctivitis)
Read More
Pinkeye (Conjunctivitis) is the inflammation (usually redness and/or swelling) of the thin tissue covering the white part of the eye and the inside of the eyelids.
There are several kinds of pinkeye, each with its own set of symptoms, including:
- Bacterial
- Red or pink, itchy, painful eye(s).
- More than a tiny amount of green or yellow discharge.
- Infected eyes may be crusted shut in the morning.
- May affect one or both eyes.
- Viral
- Pink, swollen, watering eye(s) sensitive to light.
- May affect only one eye.
- Allergic
- Itching, redness, and excessive tearing, usually of both eyes.
- Chemical
- Red, watery eyes, especially after swimming in chlorinated water.
- Immune-mediated, such as that related to a systemic disease, like Kawasaki disease.
It is helpful to think of pinkeye like the common cold. Both conditions may be passed on to other children but resolve without treatment. Pinkeye generally results in fewer symptoms of illness than the common cold.
The best method for preventing the spread of pinkeye is good hand hygiene.
Learn more about Conjunctivitis.
Sore Throat
Read More
The terms sore throat, strep throat, and tonsillitis often are used interchangeably.
However, they are not the same thing.
Tonsillitis refers to tonsils that are inflamed.
Strep throat is an infection caused by a specific type of bacteria, Streptococcus.
When your child has a strep throat, the tonsils are usually very inflamed, and the inflammation may affect the surrounding part of the throat as well.
To some extent, the symptoms of strep throat depend on the child’s age.
- Infants may have only a low fever and a thickened or bloody nasal discharge.
- Toddlers may also have a thickened or bloody nasal discharge with a fever. Such children are usually quite cranky, have no appetite, and often have swollen glands in the neck. Sometimes toddlers will complain of tummy pain instead of a sore throat.
- Children over age three are often more ill and may have a painful throat, fever over 102 degrees Fahrenheit (38.9 degrees Celsius), swollen glands in the neck, and pus on the tonsils.
It’s important to distinguish a strep throat from a viral sore throat because strep infections are treated with antibiotics.
Most pediatric offices perform rapid strep tests that provide findings within minutes. If the rapid strep test is negative, your doctor may confirm the result with a throat culture. A negative test means that the infection is presumed to be due to a virus.
Other causes of sore throats are viruses and may only cause inflammation of the throat around the tonsils and not the tonsils themselves.
In infants, toddlers, and preschoolers, the most frequent cause of a sore throat is a viral infection. No specific medicine is required when a virus is responsible, and the child should get better over a seven- to ten-day- period.
Often, children who have sore throats due to viruses also have a cold at the same time. They may develop a mild fever, too, but they generally aren’t very sick.
If your child has a sore throat that persists (not one that goes away after their first drink in the morning), whether or not it is accompanied by fever, headache, stomach ache, or extreme fatigue, you should call us.
That call should be made even more urgently if your child seems extremely ill or if they have difficulty breathing or extreme trouble swallowing (causing them to drool).
Learn more about sore throats.
Learn more about how much fever and pain medicine to give your child.
Ear Infections
Read More
Typical ear infections in children begin with either a viral infection or unhealthy bacterial growth.
Children are more prone to these problems because the passages in their ears are narrower, shorter, and more horizontal than the adult versions. And, since it’s easier for germs to reach the middle ear, it’s also easier for fluid to get trapped there.
Symptoms of an ear infection may be hard to detect. A child who constantly tugs or pulls at their ear could be exploring, or self-soothing—even though that tops the list of signs. Other symptoms include more crying than usual, especially when lying down; trouble sleeping or hearing; fever or headache; and fluid coming discharge from the ears.
Learn more about ear infections.
Learn more about how much fever and pain medicine to give your child.
Fever
Read More
If your child has a fever, they may feel warm, appear flushed, or sweat more than usual. They may also be more thirsty than usual. Some children feel fine when they have a fever. However, most will be symptomatic of the illness that is causing the fever.
A fever is usually a sign that the body is fighting an illness or infection. While it is important to look for the cause of a fever, the main purpose for treating it is to help your child feel better if they are uncomfortable or in pain.
Normal body temperature varies with age, general health, activity level, and time of day. A fever is a body temperature that is higher than normal. While the average normal body temperature is 98.6°F (37°C), a normal temperature range is between 97.5°F (36.4°C) and 99.5°F (37.5°C).
Most consider a temperature above 100.4°F (38°C) as a sign of a fever. Call your child’s pediatric healthcare provider right away if your child has a fever and:
- looks very ill, is unusually drowsy, or is very fussy;
- has been in a very hot place, such as an overheated car;
- has other symptoms, such as a stiff neck, severe headache, severe sore throat, severe ear pain, an unexplained rash, or repeated vomiting or diarrhea;
- has immune system problems,
- has had a seizure;
- is younger than three months (12 weeks) and has a temperature of 100.4°F (38.0°C) or higher; or
- their fever rises above 104°F (40°C) repeatedly for a child of any age.
Also, call if:
- your child still “acts sick” once the fever is brought down;
- your child seems to be getting worse;
- their fever persists for more than 24 hours in a child younger than 2 years; or
- their fever persists for more than three days (72 hours) in a child 2 years of age or older.
Learn more about fever in children.
Learn more about how much fever and pain medicine to give your child.
Sick Exams
Read More
If your child is sick, injured, or struggling developmentally or emotionally—please call!
Sometimes, it can be hard to tell how sick your child is. We can advise you if their symptoms warrant a visit to our office.
You can also use the KidsDoc Symptom Checker to help you decide.
Learn more about how much fever and pain medicine to give your child.
Immunizations
Read More
Published by the Centers for Disease Control & Prevention (CDC), these downloadable PDFs show the 2021 Recommended Immunizations for Children.
On-time vaccination throughout childhood is essential because it helps provide immunity before children are exposed to potentially life-threatening diseases. Vaccines are tested to ensure that they are safe and effective for children to receive at the recommended ages.
Learn more about:
Asthma
Read More
Asthma is the most common chronic disease affecting children worldwide. About 1 in 12 children in the United States have asthma, according to the Centers for Disease Control & Prevention (CDC).
There is no cure for asthma, but there are ways to control it.
Learn more about asthma and common triggers for it, such as:
- allergens,
- viral colds,
- insects,
- animals,
- pollutants,
- weather,
- exercise, and
- stress.
Allergies
Read More
Allergies are reactions that are usually caused by an overactive immune system. These reactions can occur in a variety of organs in the body, resulting in diseases such as asthma, hay fever, and eczema.
In an allergic reaction, the immune system overreacts and goes into action against a normally harmless substance, such as pollen or animal dander. These allergy-provoking substances are called allergens.
Although allergies can trigger asthma, and asthma is often associated with allergies, they are actually two different things.
In simple terms, asthma is a chronic condition originating in the lungs, whereas allergies describe reactions that originate in the immune system and can affect many organs, including the lungs.
Allergies can result in various types of conditions. Some are easy to identify by the pattern of symptoms that invariably follows exposure to a particular substance; others are more subtle and may masquerade as other conditions.
Learn more about allergies.
COVID-19
Read More
COVID-19
Doctors and researchers continue to learn more about COVID-19 every day. Safe and effective vaccines are now available, offering hope for an end to the pandemic. Until everyone is vaccinated, however, the virus continues to spread.
Symptoms of COVID-19 range from mild to severe and generally begin two to 14 days after being exposed to the virus. Someone with these symptoms may have COVID-19:
- fever and chills
- a cough
- shortness of breath or difficulty breathing
- muscle or body aches
- headache
- sore throat
- new loss of taste or smell
- congestion or runny nose
- nausea or vomiting
- diarrhea
Although COVID-19 is a new disease, it belongs to a family of coronaviruses that usually cause illnesses like the common cold.
According to the CDC, children do not seem to be at higher risk for getting COVID-19 unless they have an underlying health condition such as obesity, diabetes, lung conditions, heart conditions, or conditions that weaken the immune system.
Learn more about what families need to know about COVID-19.
Learn more about how much fever and pain medicine to give your child.
MIS-C
You may have heard news reports about a possible connection between COVID-19 and a rare but serious health condition in children called multisystem inflammatory syndrome in children (MIS-C). Scientists worldwide, including pediatric specialists, are working together to understand MIS-C and how best to diagnose and treat it.
Children with MIS-C are very ill with a fever for 24 hours or more, have inflammation in their bodies, and problems with many organs, such as the intestines, heart, brain, lungs, skin, and kidneys. Contact your child’s pediatric healthcare provider right away if you notice any of these symptoms:
- fever (100.4 degrees Fahrenheit or higher) lasting 24 hours or more
- abdominal pain, diarrhea, or vomiting
- neck pain
- rash or changes in skin color
- bloodshot eyes
- seems extra tired
- shortness of breath
- pain or pressure in the chest that doesn’t go away
- becoming confused
- unable to wake up or stay awake
- bluish lips or face
While MIS-C sounds frightening and is serious, remember that it’s still rare.
Learn more about COVID-19 and MIS-C.
Help Children Cope with the COVID-19 Pandemic
The ongoing stress, fear, grief, isolation, and uncertainty created by the COVID-19 pandemic can wear anyone down, but many children and teens have had a tough time coping. At the same time, many families have been separated from loved ones and caregivers, including grandparents, who may serve as vital sources of support.
As more people get COVID-19 vaccines, there is growing hope that the pressures of the pandemic will ease. But, the struggles and losses will likely continue to affect families for some time to come. Continue to check in with your child often and watch and listen for signs they are struggling. And, remember that your pediatric healthcare provider is available to help.
Invite your child to talk about how they are feeling. Feeling depressed, hopeless, anxious, and angry may be signs they could benefit from more support during this difficult time.
Learn more about how to help your child cope during the COVID-19 pandemic.
RSV
Read More
Almost all children will have a respiratory syncytial virus (RSV) at least once before they are 2 years old. For most healthy children, RSV is like a cold. But, some children get very sick.
RSV is one of the many viruses that cause respiratory illness—illnesses of the nose, throat, and lungs. It occurs in the late fall through early spring months.
Typically, RSV causes a cold, which may be followed by bronchiolitis or pneumonia. Symptoms generally last an average of five to seven days. RSV symptoms are typically at their worst on days three through five.
Fortunately, almost all children recover from an RSV infection on their own. However, some children with RSV may be at increased risk of developing a bacterial infection, such as an ear infection.
RSV is contagious and spreads just like a common cold virus. It enters the body through the nose or eyes, usually from:
- direct person-to-person contact with saliva, mucus, or nasal discharge;
- unclean hands (RSV can survive 30 minutes or more on unwashed hands.); or
- unclean objects or surfaces (RSV can survive up to six hours on surfaces, toys, keyboards, doorknobs, etc.).
There is no cure for RSV, and medications, like steroids and antibiotics, do not help.
Learn more about RSV.
Learn more about how much fever and pain medicine to give your child.
Eczema
Read More
Eczema (also called atopic dermatitis) is an ongoing skin problem that causes dry, red, itchy skin and is caused by problems with the skin barrier.
Both genetics and the environment play a role in eczema. It often runs in families and tends to occur with other allergic conditions, such as asthma and allergic rhinitis (hay fever and seasonal allergies). Many children with eczema also have food allergies, but foods themselves do not cause eczema.
Eczema rashes can be different for each child. They can be all over the body or in just a few spots. The eczema rash often worsens at times and then gets better. Where the rashes develop may change over time:
- In babies, eczema usually starts on the scalp and face. Red, dry rashes may show up on the cheeks, forehead, and around the mouth. Eczema usually does not develop in the diaper area.
- In young, school-aged children, the eczema rash is often in the elbow creases, on the backs of the knees, on the neck, and around the eyes.
Children with eczema are more prone to skin infections, but eczema is NOT contagious.
Learn more about eczema and how to treat and control it.
Summertime Rashes
Read More
Protecting your child’s skin is a year-round concern, but it’s especially important in the summer months when so much skin is exposed and vulnerable.
Fortunately, many summertime rashes clear up quickly on their own. Be sure to talk with your pediatric healthcare provider about any rash that you’re unsure about—especially if:
- you don’t know what caused it,
- it’s making your child miserable,
- it doesn’t clear up quickly,
- it shows signs of infection, or
- it’s accompanied by any shortness of breath.
The following are 12 common summertime skin rashes seen in children:
- Heat Rash
- Poison Ivy & Other Plant Rashes
- Eczema
- Insect Bites & Stings
- Impetigo
- Swimmer’s Itch
- Cutaneous Larva Migrans (Sandworms)
- Folliculitis (Hot Tub Rash)
- Molluscum Virus
- Juvenile Plantar Dermatosis (Sweaty Sock Syndrome)
- Tinea (Ringworm)
- Hand, Foot & Mouth Disease
Learn more about how to prevent, identify, and soothe these skin problems.
Sports Physicals
Read More
To make life easier (and what parent wouldn’t like that), the American Academy of Pediatrics (AAP) recommends asking to have a sports physical when scheduling your child’s next routine well-child visit.
Why should all kids benefit from a sports physical during a well-child visit?
The answer is simple: All kids are athletes―the high school soccer player, the junior high performer in the school musical, and the skateboarding middle schooler down your block.
You don’t have to play an organized sport to be an athlete. Many children participate in physically demanding activities like snowboarding, skiing, jogging, climbing, and hiking. Other children are not physically active at all.
Seeing your pediatric healthcare provider for routine well-child visits and sports physicals helps keep your child’s medical records and health history up to date. And, they can ensure your child is caught up on immunizations and discuss any concerns in a confidential setting.
The AAP recommends making appointments at least 6-8 weeks before starting a season to give time for any additional evaluation or new treatments.
Learn more about sports physicals.
Developmental Screenings
Read More
The American Academy of Pediatrics (AAP) recommends that children receive screening for development at nine, 18, and 24 or 30 months and for autism at 18 and 24 months. Screening also can be done whenever a parent or pediatric healthcare provider has concerns.
You can easily track and celebrate your child’s development with free milestone checklists from the Centers for Disease Control & Prevention (CDC). You can also download and use the free Milestone Tracker app for iPhone or Android.
The CDC also maintains a free library of photos and videos—Milestones in Action— to help you identify your child’s important developmental milestones.
Talk, read, sing and play with your child every day. The CDC’s “Amazing Books” are fun for children and show you what to look for as your child grows.
- Age 1: Baby’s Busy Day
(en Español, Un día ocupado del bebé) - Age 2: Where is Bear?
(en Español, ¿Dónde Está Osito?) - Age 3: Amazing Me
(en Español, Soy Maravilloso)
As a parent, you know your child best. If your child is not meeting the milestones for their age, or if you think there could be a problem with the way your child plays, learns, speaks, acts, and moves—talk to your child’s pediatric healthcare provider and share your concerns.
Don’t wait. Acting early
can make a real difference!
Learn more about how to act on developmental concerns.
Emotional Problems
Read More
Children’s temperaments vary, and they can be quite different in their ability to cope with stress and day-to-day life. Some are easygoing and adjust well to new situations. Others are thrown off balance by changes in their lives.
Learn more about emotional problems (such as panic, anxiety, OCD, depression, bipolar disorder, and eating disorders).
Disruptive Behavior
Read More
Disruptive behavior disorders are among the easiest to identify of all coexisting conditions because they involve behaviors that are readily seen, including:
- temper tantrums,
- physical aggression,
- argumentativeness,
- stealing, and
- other forms of defiance, or
- resistance to authority.
These disorders, which include Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD), often first attract notice when they interfere with school performance, family, or friendships; and they frequently intensify over time.
ODD is defined in the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) as including persistent symptoms of “negativistic, defiant, disobedient, and hostile behaviors toward authority figures.”
CD is a more extreme condition than ODD. Defined in the DSM-IV as “a repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate social rules are violated.”
ADHD
Read More
Attention deficit hyperactivity disorder (ADHD) is a developmental disorder that affects the behavior, attention, and learning of children.
Children with ADHD have behavior problems that are so frequent and severe that they interfere with their ability to live normal lives.
ADHD includes 3 groups of behavior symptoms: inattention, hyperactivity, and impulsivity.
Learn more about ADHD at Understood.com.
Anxiety
Read More
Anxiety disorders are often more difficult to recognize than disruptive behavior disorders because the former’s symptoms are internalized—often only existing within the mind of the child rather than in outward behaviors.
An anxious child may be experiencing guilt, fear, or even irritability, and yet escape notice by a parent or teacher. Only when symptoms are expressed in actual behavior, such as weight loss, sleeplessness, or refusal to attend school, will they attract the attention they need.
Please ask your child’s pediatric healthcare provider to talk with your child directly if you suspect the presence of persistent anxiety.
Children with anxiety may have worries that are clear-cut, often focusing on specific situations or thoughts. They may seem tense, irritable, tired, or stressed out. They may not sleep well, and may even experience brief panic attacks—involving a pounding heart, difficulty breathing, nausea, shaking, and intense fears—that occur for no apparent reason.
Learn more about anxiety.
Additional information from HealthyChildren.org:
Additional information from the American Academy of Child & Adolescent Psychiatry (AACAP):
Obesity
Read More
Various factors can influence the likelihood of a child becoming overweight. Obesity is usually defined as more than 20 percent above ideal weight for a particular height and age.
Obesity is a serious health concern that can put children at risk for complications that can affect their health in the short and long term. Scientists have found obesity to be a risk factor for severe illnesses. It can raise the risk for problems such as diabetes, hypertension, chronic joint pain, sleep apnea, and psychosocial stress such as bullying and low self-esteem. We also know that children with obesity tend to be more likely to have obesity later in life. However, it’s never too late to make healthy and positive changes for your family!
Body Mass Index or BMI is a calculated measurement of someone’s weight in relation to their height. It serves as a quick estimate of body fat. It is puts people in weight categories such as underweight, overweight, and obese.
We know that children are constantly growing, and do so at different rates. In addition, male and female children have differences in body fat distribution, within a range of normal body shapes and sizes. So, instead of just using the calculated BMI number as is done with adults, BMI percentiles consider children’s growth and development to figure out if they are within their healthy weight range.
Learn more about Body-Mass Index (BMI) in Children.
Children below the 5th percentile could have a nutritional shortfall—either not taking in enough calories or burning up more calories than they are getting, or both. Likewise, children above the 85th percentile are likely, but not always, getting too many calories in their diet, not burning up enough calories through physical activity or both. Although less common, some medical conditions can cause children to gain or lose weight more easily.
If your child falls outside of the 5th and 85th BMI percentiles, talk with your pediatric healthcare provider about the best treatment options tailored to their individual needs.
Every family should aim to incorporate a balanced and nutritious diet and daily exercise into a child’s routine.
Urgent Care Concerns
Read More
When your child suddenly becomes sick or hurt, it can be difficult to tell whether urgent or emergency care is the best choice. Try to remain calm and recognize the difference.
Remember—you can always call our office!
In fact, it should be the first step once you’ve come to the conclusion that your family is dealing with a non-emergency situation.
If your pediatric healthcare provider is unable to see you but believes your child should be examined, they will advise you on the most appropriate place for your child to receive care and how quickly your child should be seen.
Situations that warrant care for illness or injury, but not emergency care:
- Minor burns
- Earache or ear infection
- Pink eye
- Potential urinary tract infection (UTI)
- Sore throats and potential strep throat
- Rashes and mild skin infections
- Gastrointestinal illnesses, such as vomiting and diarrhea with mild dehydration
- Simple wounds
- Foreign objects in ears and noses Colds and coughs
- Allergies
Learn more at HealthyChildren.org:
*Information on this page is sourced from HealthyChildren.org, the American Academy of Pediatrics (AAP), the American Academy of Child & Adolescent Psychiatry (AACAP), the Society of Pediatric Dermatology (SDP), and the Centers for Disease Control & Prevention (CDC).
Information found on the PremierPlusPediatrics.com website should not be used as a substitute for the medical care and advice of your pediatric healthcare provider. Variations in treatment recommendations are based on individual facts and circumstances.
Last updated: 05/03/2021.